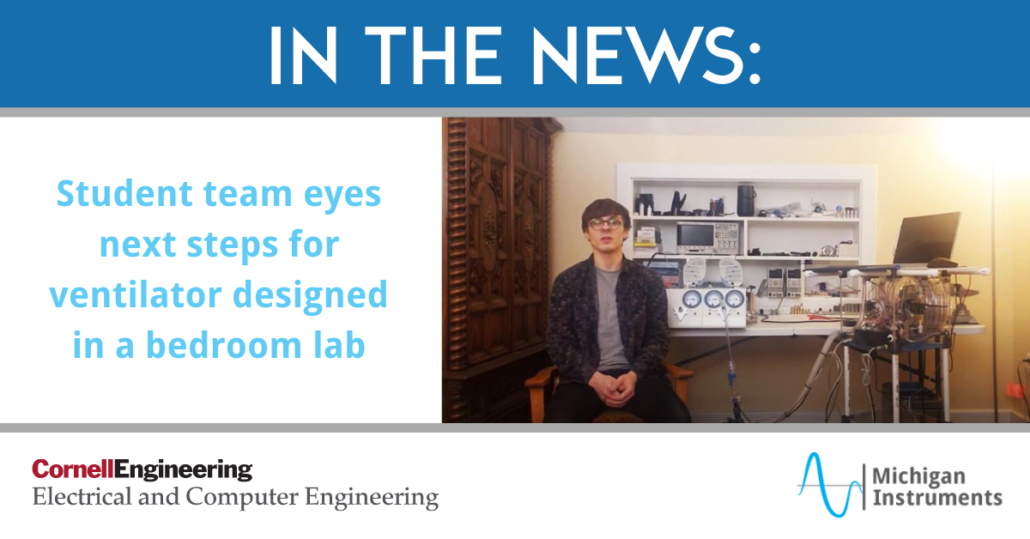
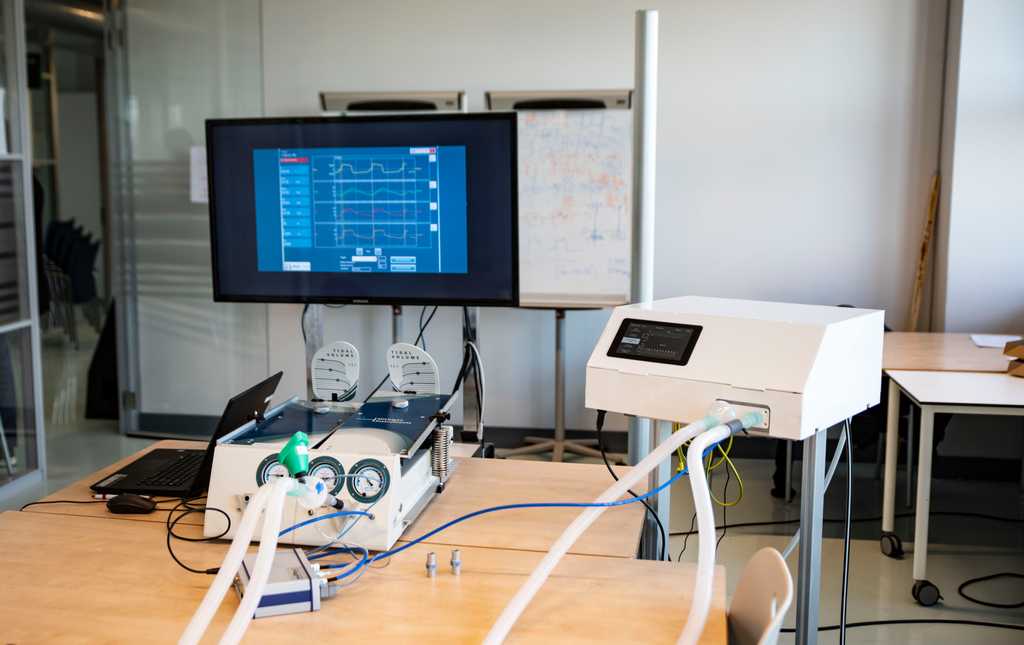
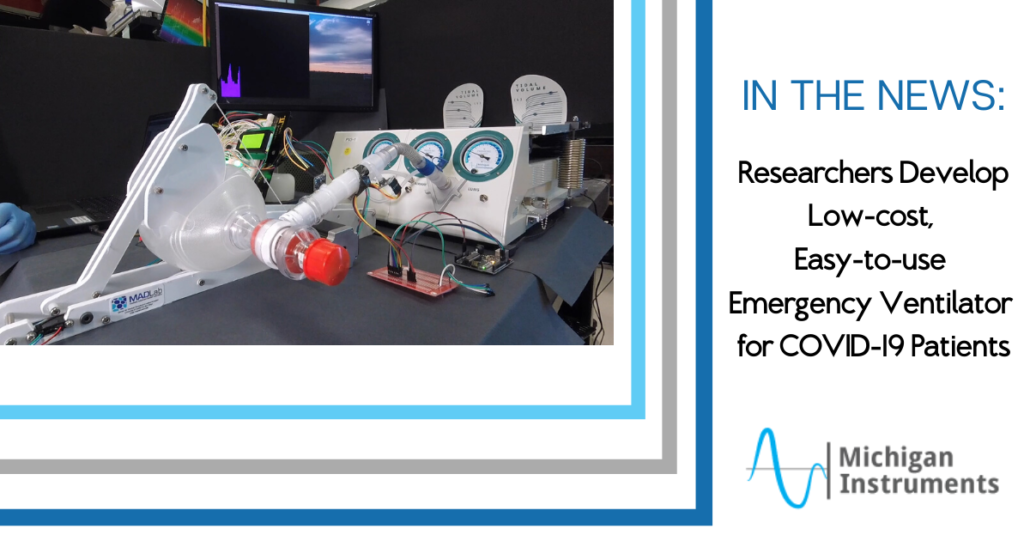
In these recent months of the COVID-19 crisis, many companies and institutions have taken on ventilator design and manufacturing for the first time. With our long history of involvement with researchers and ventilator manufacturers, Michigan Instruments has played a role in many of these recent efforts, providing our calibrated lung simulators (TTL and PneuView) to auto manufacturers, electronics companies, Universities, and even NASA to support their development and manufacturing efforts. One of the things that we know at Michigan Instruments, as do most medical professionals involved in mechanical ventilation, is that not just any ventilator can be used on any patient.
Ventilators range in complexity from very simple emergency units that are meant for short-term use in the pre-hospital or field setting, to long-term care ventilators that are used in homes or institutions to support patients with chronic breathing issues, to critical care ventilators used in ICU’s to deal with acute illness, severe trauma, or post-surgical cases. These units can have very different features and capabilities. All ventilators are not created equal, and that’s intentional.
The virus that causes COVID-19 is designated severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The major morbidity and mortality from COVID-19 is largely due to acute viral pneumonitis that evolves to acute respiratory distress syndrome (ARDS). Patients that develop ARDS will often end up on a ventilator in the ICU. These patients can be difficult to ventilate, requiring high levels of oxygen and relatively high ventilating pressures to move adequate breath volumes in and out of the lungs. And that’s the issue. Not just any ventilator will meet the needs of these patients.
As mentioned above, Michigan Instruments has been involved in many of these recent efforts to ramp up ventilator production in response to the COVID-19 pandemic. Our lung simulators are being used all over the world. We wouldn’t presume to know exactly what kinds of ventilators will work best to treat these COVID-19 patients, but we believe there are some reasonable basic features and minimal capabilities that should be incorporated into the ventilators being developed and built to deal with this crisis.
- Oxygen %: Adjustable from 21 to 100% (either built-in or adjustable external O2/Air blender)
- Respiratory Rate: Up to 40 breaths per minute (BPM)
- Tidal Volume: 100 to 1000mL
- Pressure Limit: Up to 60 cmH2O
- PEEP: Up to 15 cmH2O
- Alarms: Low Pressure, Disconnect, High Pressure, Loss of O2 Source
- Other Features: Synchronized to patient effort; high sensitivity to patient effort; sine or decelerating flow waveform; dual-limb breathing circuit with adequate filtration of inhaled and exhaled gases
Note: These features are the opinion of the technical specialists at Michigan Instruments and should not be taken as official guidelines or requirements. In an emergency situation, we believe that almost any mechanical ventilator will be superior to no support or prolonged use of a manual resuscitator.
The Michigan Instruments TTL Training Test Lungs and PneuView Systems have played an invaluable role in the effort to meet the need for reliable, tested mechanical ventilators. Our products and our expertise have been called upon by old and new partners around the world during this pandemic crisis. Whether your role is in development, design, or manufacture of ventilators, we’ve got the lung simulator products that are tried, trusted, and often specified to meet your testing needs.
Learn more about our Lung Simulator Devices here or contact us today for more information!