The rapid advancement of medical technology has revolutionized healthcare, offering promising solutions for diagnosis, treatment, and patient care. Many of these innovations, from wearable devices that monitor vital signs to lung simulators, have the potential to enhance patient outcomes and improve overall public health.
However, the benefits of these innovations are coupled with significant ethical dilemmas due to the delicate balance between technological progress and ensuring patient privacy with protection of data security in healthcare.
HIPAA Privacy: Safeguarding Patient Information
Medical and other personally identifiable health information is private, and as such, it must be protected! Most Americans want to know who has access to their health information. It’s for these reasons that the Health Insurance Portability and Accountability Act, better known as HIPAA, exists.
There are two different sets of HIPAA regulations:
- The Privacy Rule: A Federal law that gives you rights over your health information and sets rules and limits on who can look at and receive your health information. The Privacy Rule applies to all forms of individuals’ protected health information, whether electronic, written, or oral.
- The Security Rule: A Federal law that requires security for health information in electronic form.
What Information Is Protected by HIPAA?
According to HHS.gov, the following information is protected by HIPAA regulations:
- Protected Health Information (or PHI) is any individually identifiable health information that is collected from an individual, and is transmitted, received, created and/or maintained, in any form or medium, by a company who is required to follow HIPAA.
- Information documented in your medical record by doctors, nurses, and other health care providers.
- Conversations that any member of your care team discusses with others involved in your treatment.
- Health insurance plans’ electronic data about their insured patients.
- Billing information at healthcare facilities where you receive care.
Understanding HIPAA Regulations
HIPAA plays a critical role in addressing the ethical challenges surrounding medical technology, patient privacy, and how patient’s health information can be used or disclosed. So, what does it protect, and who is unable to access Protected Health Information?
Covered Entities Must Follow HIPAA Regulations
Covered entities are companies or entities who must follow HIPAA laws. This would also include business associates of covered entities. This is applicable if the business associate has access to the patient information and uses the information to perform a function on behalf of the covered entity.
Examples of business associates would include contractors, subcontractors, and other outside persons and companies that are not employees of a covered entity. There must be a written agreement, between the covered entity and business associates, that specifically outlines what the business associate has been engaged to do and requires that they also protect PHI and comply with the HIPAA rules.
Covered entities include:
- Health Plans: Health insurance companies, HMOs, company health plans, and government programs that pay for health care, such as Medicare and Medicaid.
- Most Health Care Providers: Those that conduct certain business electronically, such as electronically billing your health insurance—including most doctors, clinics, hospitals, psychologists, chiropractors, nursing homes, pharmacies, and dentists.
- Health Care Clearinghouses: Entities that serve as a middleman, of sorts, to process nonstandard health information they receive from another entity into a standard (i.e., standard electronic format or data content), or vice versa.
Examples of Entities That Are Not Bound by HIPAA Laws
Some entities or businesses are not required to adhere to HIPAA laws and guidelines. These entities may still collect and maintain sensitive health information about you, so it’s important to know what information they have and what they can share.
Examples of organizations that do not have to follow the Privacy and Security Rules include:
- Life insurers
- Employers
- Worker compensation carriers
- Most schools and school districts
- Many state agencies like child protective service agencies
- Most law enforcement agencies
- Many municipal offices
Technological Advances and Challenges With HIPAA
The entire world seems to be going digital, and healthcare is no exception! With the widespread adoption of digital health technologies and technological advances being made, there are new challenges associated with tech and HIPAA compliance.
With the addition of mobile health apps, remote monitoring devices, and telemedicine platforms, the collection and sharing of health information has expanded greatly. While these technologies offer convenience and accessibility, they also increase the risk of data breaches and privacy violations if not properly secured and regulated.
The Need for Advancements in Technology
With an abundance of health information being gathered in new ways, it goes without saying that all of this data can be used for technological advancements in a way that has not been previously available:
- Personalized Medicine: Patient data, such as genetic information, medical history, and lifestyle factors, can be used to tailor treatments and medications to individual patients. This approach, known as personalized or precision medicine, aims to improve treatment efficacy and reduce adverse effects by considering each patient’s unique characteristics.
- Predictive Analytics: Analyzing patient data can help predict and prevent diseases before they manifest clinically. Machine learning algorithms can identify patterns and risk factors, allowing healthcare providers to intervene early and implement preventive measures.
- Clinical Research and Drug Development: Patient data is crucial for clinical research and drug development. Researchers use anonymized patient data to study disease patterns, test new treatments, and assess medication safety and efficacy.
- Technological Advancements: Patient data and using patients for research is critical for the creation of new, life-saving technologies However, using this data to support further research and reveal efficacy rates can pose ethical challenges related to patient privacy.
While these advancements offer significant benefits, they also raise ethical considerations related to patient privacy, consent, and data security in healthcare. It’s essential to balance the potential benefits of using patients’ data for medical innovations with protecting their rights to ensure data privacy and confidentiality.
Regulatory frameworks like HIPAA provide guidelines and standards to safeguard patient information and uphold ethical principles in healthcare data use.
Privacy Concerns Associated with Medical Technology
Because advancements in medical technology often require access to a wide range of patient information, including medical history, genetic data, lifestyle habits, and treatment outcomes there are undoubtedly concerns about privacy violations.
Revealing Data Could Get Into the Wrong hands
For example, the collection and analysis of genetic data can reveal sensitive information about an individual’s predisposition to certain diseases or conditions. If this data is not adequately protected, it could be exploited for discriminatory purposes by employers, insurers, or other entities.
Similarly, tracking patient behavior through wearable devices or digital health apps could lead to privacy breaches if the data is accessed or shared without proper consent.
Data Could Be Breached, Causing Mistrust Between Patient and Medical Entities
Medical data in a research setting requires the integration of data from multiple sources, such as electronic health records, wearables, and social determinants of health. All of this data collection creates complex data ecosystems that increase the risk of unauthorized access or data breaches. Without proper security measures, the misuse or breach of this data could jeopardize patient privacy and trust.
Clearly, a delicate balance exists between the need for data-driven innovations and respecting patients’ privacy rights. Healthcare organizations must implement data protection strategies, including encryption, access controls, audit trails, and regular cybersecurity audits.
Additionally, transparent communication with patients about data collection, usage, and sharing practices is essential to building and maintaining trust in the digital healthcare landscape.
Exploring Health Innovations with Michigan Instruments
While advancements in medical technology offer tremendous potential for improving patient care and outcomes, they also pose significant ethical challenges related to privacy and data protection.
By upholding ethical standards, complying with regulations like HIPAA, and adopting responsible data governance practices, Michigan Instruments and the healthcare industry as a whole can harness the power of technology while safeguarding patient privacy and trust.
The Future of Health Begins Here
Our commitment to advancing technology in healthcare extends beyond compliance with the legal requirements of HIPAA. We prioritize ethical standards and patient privacy in all our endeavors, striving to set a higher bar for responsible data use and innovation.
Our dedication is not just to meet existing standards but to exceed them, ensuring that every technological advancement we pursue is ethically sound and contributes positively to patient care.
We invest significant time, energy, and resources into developing cutting-edge solutions that enhance health outcomes both now and in the future. By harnessing the power of technology, we aim to revolutionize healthcare delivery, improve treatment effectiveness, and ultimately save lives.
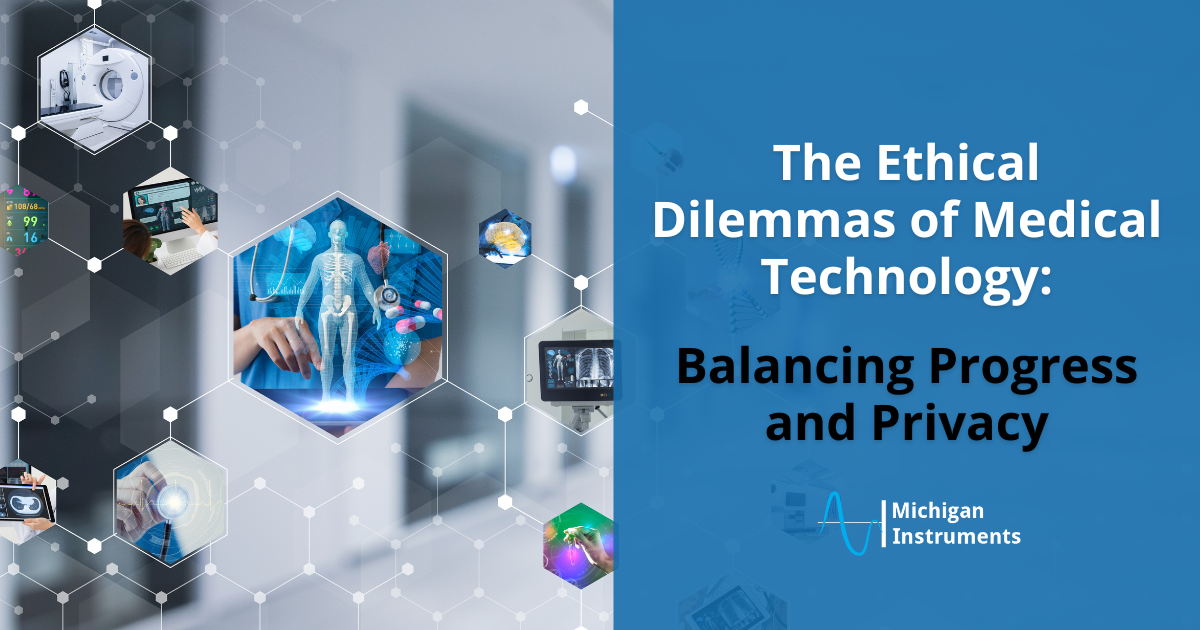
To experience the transformative impact of our innovations firsthand, we invite you to request a quote for our range of devices, including lung simulation products and mechanical CPR devices such as Thumper and Life-Stat. These devices are designed to optimize patient care, provide critical support during medical emergencies, and empower healthcare professionals with the tools they need to deliver exceptional care.
Contact us today to learn more about how our advanced technology solutions can elevate your healthcare practice and contribute to better patient outcomes.