In recent years, the integration of Artificial Intelligence (AI) into medical devices has shown tremendous promise. AI-powered medical devices have the potential to revolutionize diagnostics, treatment planning, and patient care.
However, before diving headfirst into the realm of AI medical tools, it’s essential to consider the potential drawbacks that come with these advancements.
In this blog, we’ll delve into some of the significant concerns surrounding AI medical tools—helping you make an informed decision for your healthcare practices.
1. Reliability and Accuracy
AI medical tools heavily rely on large datasets and complex algorithms to make decisions. While they have shown impressive accuracy rates in various studies, no AI system is infallible.
Medical decision-making involves complex variables, and errors can occur due to biases in the training data, algorithmic limitations, or even technical glitches. Relying solely on AI tools without proper human oversight could potentially compromise patient safety and care quality.
2. Lack of Human Judgment
Medicine is as much an art as it is a science. Physicians bring not only their knowledge, but also their intuition and empathy to the table. AI medical tools lack the human touch that comes with a doctor’s ability to understand nuanced patient histories, emotional states, and subtle physical cues.
Relying solely on AI tools might lead to missed diagnoses or inappropriate treatment recommendations in situations that require a deeper understanding of the patient’s life circumstances and emotional state.
3. Data Privacy and Security
AI medical tools thrive on massive amounts of patient data. This raises significant concerns about data privacy and security. Healthcare data is highly sensitive and protected by various regulations, like HIPAA.
The use of AI tools necessitates the sharing of this data with third-party vendors or cloud services, potentially putting patient confidentiality at risk. A breach in data security could have severe legal and ethical implications.
4. Complex Implementation and Training
Integrating AI medical tools into existing healthcare systems isn’t a seamless process. It requires substantial investments in infrastructure, training, and IT support—which isn’t always possible for smaller or more rural healthcare facilities.
Physicians and medical staff need to be adequately trained to understand and use these tools effectively. If not implemented correctly, AI tools can lead to confusion, resistance, or even misuse, negatively impacting patient care.
5. Dependency and Skill Erosion
Relying heavily on AI medical tools could lead to a decline in the medical community’s core skills. As doctors become more dependent on AI for diagnoses and treatment planning, their ability to critically analyze cases and make independent decisions might diminish.
Over time, this could lead to a generation of healthcare professionals who are skilled at operating AI tools but lack the essential clinical acumen that distinguishes great doctors from good ones.
The Michigan Instruments Approach
The integration of AI into the medical field undoubtedly offers exciting possibilities. While AI medical tools can streamline processes, aid in early detection, and enhance patient outcomes, they cannot replace the nuanced understanding and empathetic care that only a human medical professional can offer.
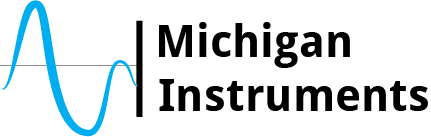
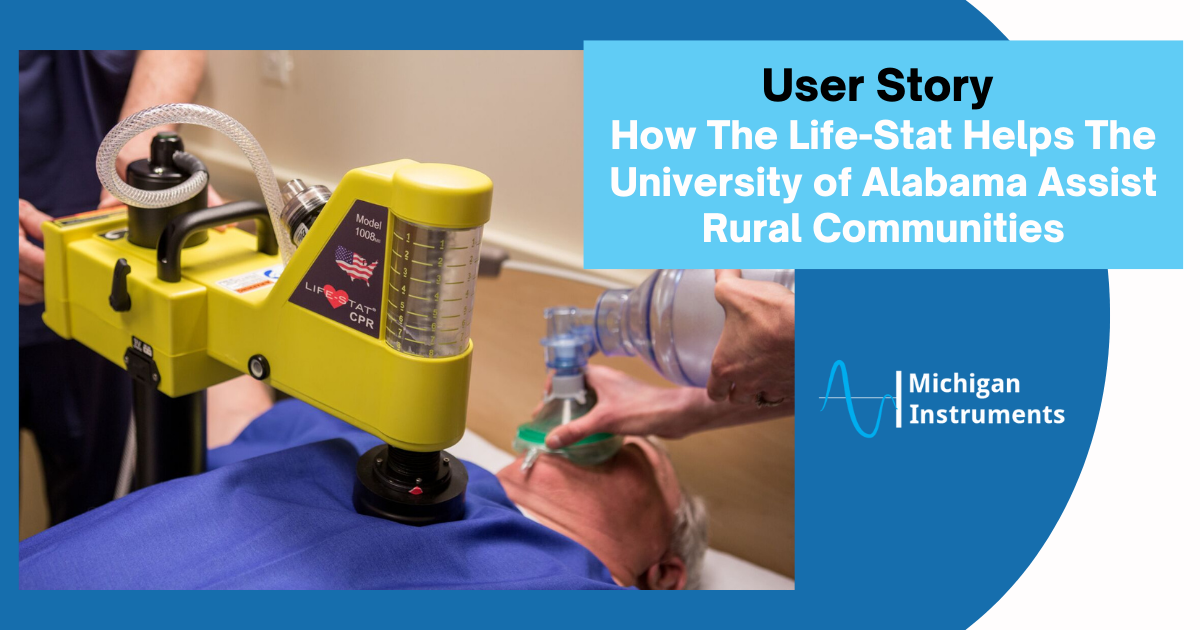
Bridging this gap, our automated CPR machines provide a happy medium between manual and AI medical treatments. They integrate seamlessly into emergency response scenarios, allowing healthcare providers to focus on life-saving interventions without sacrificing the quality of care during cardiac events.
By keeping the medical professional at the helm of decision-making, these machines offer an optimal blend of manual expertise and automated efficiency. They also enhance the safety and well-being of the rescuers, allowing them to be better positioned and less prone to injury.
As we navigate the complex landscape of AI in healthcare, it’s important to remember that technology should be a tool, not a replacement, for human skill and compassion.
To demo an automated CPR machine for your medical facility, contact us today!