This year, May 21st – May 27th is National EMS Week. This week is dedicated to celebrating EMS employees and the important part they play in our nation’s communities to help save lives.
In light of this annual event, we would like to acknowledge the importance of proper education and technology for your EMTs.
Below are the different ways to provide your EMTs with continuous education, and all the benefits that they provide.
1. Understand Why Continuing Education is Important
All EMS organizations should offer continuing education within their facility, or in partnership with other healthcare organizations. However, continuing education for EMTs offers more benefits than just filling a requirement to maintain certifications.
There are several benefits to providing your EMTs with education indefinitely, such as:
More Effective and Efficient Treatment
Keeping up with the latest medical information and technology allows EMS teams to provide better treatment for their patients.
New practices and technologies (like ours) can save emergency medical professionals time by treating patients with methods that may not have been previously available.
Reduced Risk
Continuing education also reduces liability risk from malpractice or wrongful death. Failure to be consistent with education can result in incorrect treatment, misdiagnosis, or other life-threatening mistakes.
Networking Opportunities
In-person education programs, such as classes and conferences, allow EMS administrators to build connections and grow their network. Forming relationships in the industry can open new career paths, and create opportunities for shared knowledge.
2. Explain the Importance of Learning from Others
No matter what role you play or how long you may have been performing your job, you should never assume there isn’t more to learn—especially in healthcare. Healthcare professionals should always be willing to learn new information or gain new perspectives from others.
This also includes helping them acknowledge the value of feedback, and doing self-assessments to better understand their strengths and weaknesses.
3. Be Open to Multiple Teaching Techniques
While all of your EMTs should remain open to learning new things, they might not have the same preferred learning styles or methods.
Some learn best in a classroom-like environment, while others may prefer educational apps, medical devices, academic journals, or mentors. Keep your options open when looking for educational opportunities for your staff.
The National Association of EMS Educators offers many options for educating EMS Professionals. This is just one of the many ways to find resources that you can use to craft an educational plan for your EMTs.
4. Select Your Best Personnel for QI Leadership
In order to have an effective quality improvement (QI) program, it is understood that providers want to do a better job of providing patient care. If your QI program is successful, it will help your EMTs recognize opportunities within their patient care and encourage them to make proper corrections.
If your QI program is less successful, you may have the wrong leader and might consider making a change to ensure more effective leadership.
Enlist the help of your best and most qualified clinicians to do QI. Teach them about good culture, statistical process control, normal and special cause variation, and other improvement science concepts that drive them to improve care and be better leaders for the team.
5. Commit to Communication
One of the key reasons why things can go wrong in healthcare organizations is a lack of communication. There is a failure to communicate issues, questions or changes that would benefit the team.
When discovering concerns and/or opportunities to improve, it’s vital to share them with your staff. Encourage your team to practice continuous communication no matter what.
An operation without communication is a recipe for disaster. In an environment where everyone is working collaboratively to save lives, all aspects of communication—including addressing errors, offering constructive feedback, and updating staff on changes in practices—are of utmost importance for a successful operation.
6. Provide Your Team With Michigan Instruments’ Medical Devices
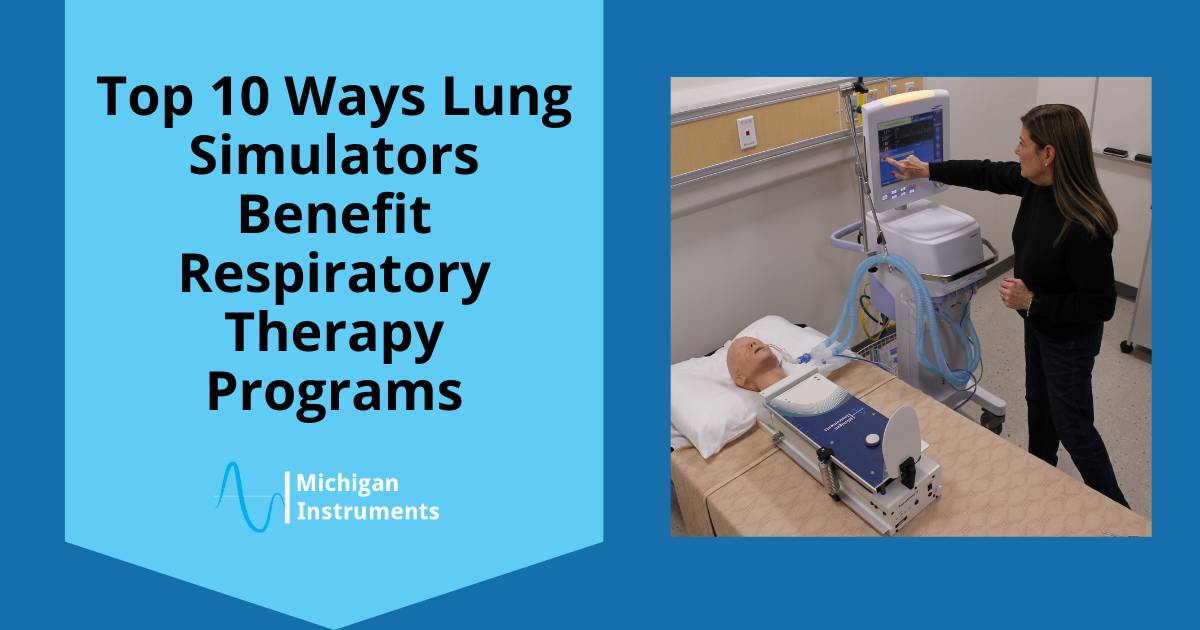
Medical technology has been known to be an avenue for effective education for many healthcare professionals—especially those who practice emergency services.
For example, our lung simulators can provide helpful training and practice for EMTs. They are fully adjustable and provide a dynamic response to therapy that accurately demonstrates how the human pulmonary system works.
In addition, we offer outstanding medical equipment, such as our automated CPR machines. These help EMS teams to be more efficient and effective.
Our Life-Stat and Thumper CPR devices support a quick and simple transition from manual to automated CPR with minimal interruption to compressions.
The Hands-Free operation of our devices and the option to automatically ventilate the patient along with chest compressions gives the EMS team more time to focus on other life-saving activities.
While very cost effective and easy to operate, these devices also can perform CPR on larger patients compared to other competing devices.
Learn More About How Our Devices Benefit Emergency Medical Practices
The importance of continuing education for your EMS team cannot be emphasized enough. However, our devices can grant your team new opportunities for both continuing education and effective patient care.
In honor of National EMS Week, contact us today for more information about why thousands of medical professionals all over the world choose Michigan Instruments.